Malnutrition is a prevalent issue among patients who are chronically hospitalized, especially those in the intensive care unit (ICU). To combat this, nutritional support through Partial Parenteral Nutrition (PPN) and Total Parenteral Nutrition (TPN) is often utilized. While both aim to provide necessary nutrients, they differ in several key aspects.
What is Parenteral Nutrition (PN)?
Parenteral nutrition (PN) refers to the administration of nutrients directly into the bloodstream, bypassing the digestive system. This method is crucial for patients who cannot obtain adequate nutrition through traditional means due to various medical conditions.
What is TPN?
Total Parenteral Nutrition (TPN) is a form of PN where all the patient’s nutritional needs are met through an intravenous (IV) line. TPN is typically used for patients who cannot consume food orally or have severe digestive issues. It involves delivering a highly concentrated solution containing all essential nutrients through a central venous catheter (CVC), usually inserted into a large vein near the heart.
What is PPN?
Key Differences Between TPN and PPN
Peripheral Parenteral Nutrition (PPN) is another form of PN, but unlike TPN, it provides only partial nutritional support. PPN is administered through a peripheral venous catheter (PVC) inserted into smaller veins, usually in the arm. The nutrient solutions in PPN are less concentrated than those used in TPN, making them suitable for short-term use and less likely to irritate the veins.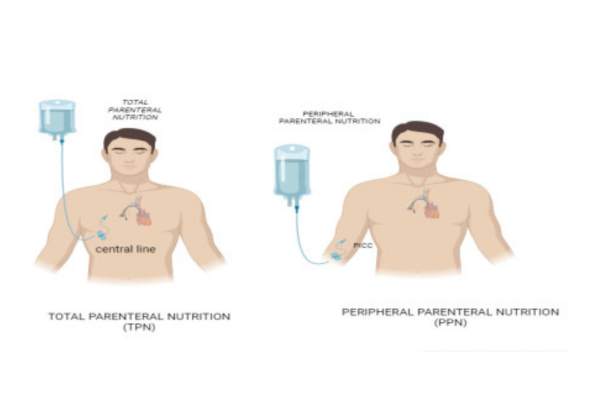
1. Administration:
- TPN: Delivered through a central venous catheter (CVC) placed in a large vein, typically in the chest or neck.
- PPN: Administered through a peripheral venous catheter (PVC) inserted into smaller veins, usually in the arm.
2. Nutrient Concentration:
- TPN: Solutions are highly concentrated, providing all necessary nutrients in a dense formulation. This requires delivery through a large vein to avoid irritation and inflammation.
- PPN: Solutions are less concentrated and more diluted, suitable for smaller peripheral veins.
3. Duration:
- TPN: Intended for long-term use, often weeks to months, and sometimes even longer depending on the patient’s needs.
- PPN: Typically used for short-term nutritional support, usually not exceeding two weeks.
4. Purpose:
- TPN: Provides complete nutritional support for patients who cannot eat or absorb nutrients through their digestive tract.
- PPN: Serves as supplementary nutrition, providing additional support when the patient can still obtain some nutrition through other means, such as a feeding tube.
5. Patient Indications:
- TPN: Suitable for patients with severe digestive issues, such as short bowel syndrome, bowel obstructions, severe pancreatitis, and those undergoing critical surgeries or treatments like chemotherapy.
- PPN: Ideal for patients with temporary digestive issues or blockages that prevent them from receiving full nutrition orally.
6. Risks and Complications:
- TPN: Higher risk of complications such as infections, liver dysfunction, and metabolic imbalances due to the more concentrated solutions and long-term use.
- PPN: Lower risk of complications, but still includes potential issues like phlebitis (vein inflammation) and infections at the catheter site.
When to Use PPN vs. TPN
PPN:
- Used when central vein access is difficult.
- Suitable for short-term or supplementary nutritional support.
- Ideal for patients with temporary nutritional needs or those recovering from surgery.
TPN:
- Used for long-term nutritional support.
- Suitable for patients with chronic conditions preventing oral intake.
- Essential for those with severe digestive tract issues or after extensive surgeries.
Monitoring and Management Both TPN and PPN
Both TPN and PPN require careful monitoring to ensure patient safety and effectiveness. Regular laboratory tests are necessary to track nutrient levels, liver function, and other critical indicators. Complications such as infections, metabolic imbalances, and catheter-related issues must be closely watched.
Final Thoughts on TPN and PPN
In conclusion, while both PPN and TPN are vital for preventing malnutrition in hospitalized patients, their use depends on the patient’s specific needs, duration of treatment, and method of administration. Understanding these differences ensures appropriate nutritional support, improving patient outcomes and quality of life.